Islet Autotransplantation for Chronic Pancreatitis
Inflammation associated with recurrent bouts of pancreatitis causes scarring and blockage of the pancreatic ducts. This produces severe chronic pain and often malabsorption because the normal function of digestive enzymes is compromised.
Pain medications, pancreatic enzyme supplementation and procedures to open blocked pancreatic ducts seem to work initially, but the improvement often do not last, leaving patients in severe pain and disabled from many activities. Removing the entire pancreas provides significant pain relief, but leaves patients severely diabetic because they no longer have pancreatic islets, which produce insulin. After removal of the pancreas, patients are completely dependent on external sources of insulin and their blood sugar can be extremely difficult to control.
|
UCSF is one of a select group of institutions offering autologous pancreatic islet transplantation as a way to minimize the severity of diabetes after the pancreas is removed. The technique involves harvesting functioning islets from the patient's own diseased pancreas and then infusing them into the portal vein, where they migrate to the liver. |
What is Chronic Pancreatitis?
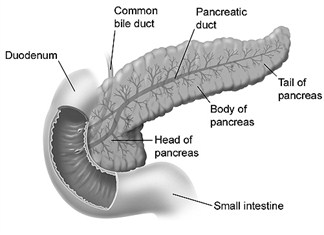 Pancreatitis is inflammation of the pancreas. The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas has two critical functions in the body:
Pancreatitis is inflammation of the pancreas. The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas has two critical functions in the body:
- The production juices that help digest food
- The production of hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body use and store energy from food.
Normally, digestive enzymes secreted by the pancreas do not become active until they reach the small intestine. However, when the pancreas becomes inflamed, as in pancreatitis, these enzymes attack and damage the the pancreas itself.
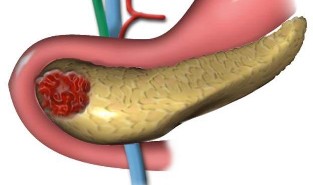
Chronic pancreatitis is inflammation of the pancreas that does not heal or improve. This causes scarring and blockage of the pancreatic ducts and chronic pain that is often difficult to relieve with medications.Patients may also develop malabsorption because the function of digestive enzymes is compromised.
Standard Treatment
Treatments range from noninvasive approaches such as pain medications and pancreatic enzyme supplementation to endoscopic procedures designed to open blocked pancreatic ducts. More invasive pain control measures may include nerve ablation or surgical procedures that attempt to improve pancreatic drainage or remove diseased portions of the organ. Most cases respond at least for a while to these interventions, but often the improvement does not last.
Insulin Dependence
Removing the entire pancreas is a last resort option in cases where standard therapy fails. This provides significant pain relief, but leaves patients severely diabetic because they no longer have pancreatic islets, which produce insulin. After removal of the pancreas, patients are completely dependent on external sources of insulin and their blood sugar can be extremely difficult to control.
Surgical Procedures
The patient undergoes a pancreatectomy to remove his pancreas. The pancreas is taken to the laboratory, where a complex procedure is used to separate the islets from the pancreatic tissue. When the islets come from the recipient's own pancreas, the isolation procedure is somewhat more rapid than with islets from a deceased donor pancreas.
Because there is no risk of rejection, the islets do not need to be as thoroughly purified and the islet yield can be lower. he islets are then infused into the patient's portal vein while he or she is still in the operating room.
Building on its expertise in organ transplantation, UCSF is the only medical center west of the Mississippi offering islet transplantation as an option for managing the diabetes that results from a treatment of last resort-removal of the diseased pancreas. The procedure is performed by Hobart Harris, M.D., M.P.H., Chief of General Surgery at UCSF, and Andrew Posselt, M.D., Ph.D., a transplant surgeon and co-director of the UCSF Pancreatic Islet Transplant Program.
The UCSF Experience
UCSF has had excellent success with the small number of patients who have so far received autologous islet transplants for chronic pancreatitis. In keeping with published findings from the few other institutions using the technique, 70 percent to 80 percent of patients have had a substantial decrease in their pain medications and 40 percent to 50 percent have been able to stop pain medications completely.
The need for supplemental insulin is a function of the numbers of islets that are harvested. Of the five patients transplanted at UCSF, three need some insulin and two do not. That 40 percent insulin-free rate is comparable to published reports.
The procedure is a good choice for highly motivated patients with a strong social support structure, including a primary care physician who can monitor their withdrawal from pain medications. Ideal patients have not yet developed diabetes from destruction of the pancreas and islets, nor have they had other pancreatic surgeries, which often produce scarring and consequently lower the islet yield. However, patients are evaluated on an individual basis.