About Us
Chief's Message
- Message from the Chief
Meet the Team
Conditions & Procedures
Patient Center
Transplant Experiences
- Patient Stories
Kidney Transplant
- New Patient Information and Forms
- Patient Referrals
Liver Transplant
- New Patient Information & Forms
- Liver Transplant Handbook
- Patient Referrals
Resources
- Helpful Links
- Organ Donation
- UCTV Transplant Videos
Clinics
UCSF Medical Center
- Kidney Transplant
- Liver Transplant
- Pancreas Transplant
Benioff Children's Hospital
- Kidney Transplant
- Liver Transplant
Other Locations
- Liver Transplant
- Kidney Transplant
Education & Training
Research
News & Events
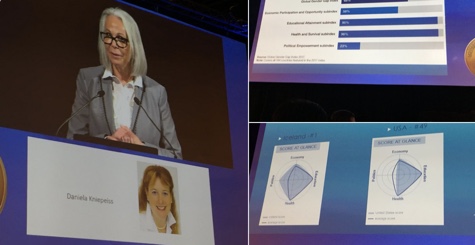
Nancy L. Ascher, M.D., Ph.D.
- Professor of Surgery
- Division of Transplant Surgery
- Isis Distinguished Professor in Transplantation
Contact Information
Education
- University of Michigan, Ann Arbor, MI, B.A., 1967-70
- University of Michigan Medical School, Ann Arbor, MI, M.D., 1970-74
- University of Minnesota, Minneapolis, MN, Ph.D., 1974-85
Residencies
- University of Minnesota, Department of Surgery, Minneapolis, MN, Surgical Internship, 1974-75
- University of Minnesota, Department of Surgery, Minneapolis, MN, Surgical Residency, 1975-77
- University of Minnesota, Department of Surgery, Minneapolis, MN, Surgical Residency, 1979-81
Fellowships
- University of Minnesota, Department of Surgery, Minneapolis, MN, Transplant Fellowship, 1981-1982
Postdoctoral Training
- University of Minnesota, Department of Surgery, Minneapolis, MN, Research Fellowship, 1977-79
Clinical Expertise
- End-Stage Kidney Disease
- Fulminant Hepatic Failure
- Hepatitis B
- Hepatitis C
- Hepatocellular Carcinoma (Liver Cancer)
- Kidney Transplantation
- Liver Cysts
- Liver Transplantation
- Living Donor Liver Transplantation
- Living Donor Kidney Transplantation
- Non-alcoholic Fatty Liver Disease
- Pediatric Kidney Transplantation
- Pediatric Liver Transplantation
- Portal Hypertension
Biography
Dr. Nancy Ascher has devoted her career to organ transplants and transplant research. Dr. Ascher completed her undergraduate and medical education at the University of Michigan, Ann Arbor. She then went on to complete a general surgery residency and clinical transplantation fellowship at the University of Minnesota.
Dr. Ascher joined the faculty of the Department of Surgery at the University of Minnesota in 1982 and was named Clinical Director of the Liver Transplant Program. She was recruited in 1988 by the UCSF Department of Surgery to build a liver transplantation program. In 1991, she was appointed Chief of Transplantation, an expanded role that included liver, kidney and pancreas transplants.
In 1993, Dr. Ascher was appointed Vice-Chair of the UCSF Department of Surgery, and in 1999 was appointed Department Chair where she served until September 2016.
Dr. Ascher has had a distinguished career of public service that includes appointments to the Presidential Task Force on Organ Transplantation and the Surgeon General's Task Force on Increasing Donor Organs. She also served as Chair of the Advisory Committee on Organ Transplantation for the Secretary of Health and Human Services from 2001 - 2005. Highly respected by her peers, Dr. Ascher was named to the list of U.S. News "America's Top Doctors," a distinction reserved for the top 1% of physicians in the nation for a given specialty.
Dr. Ascher is a Fellow of the American College of Surgeons and holds memberships in numerous other medical societies. She has taken an active leadership role in American Society of Transplant Surgeons activities and was its past-president. Dr. Ascher has published over 425 articles in medical and scientific journals. Her research interests are in hepatocyte immunogenicity, mechanisms of allograft rejection and clinical transplantation.
Research Overview
I. RECURRENT DISEASE AFTER LIVER TRANSPLANT
The NIH Liver Transplant Data Base has been extended to address the important issue of disease recurrence after liver transplantation. Although short term liver transplant results have improved markedly over the past ten years, it is apparent that disease recurrence is an important source of patient morbidity and graft loss. Long term following of greater than 1000 patients in the Liver Transplant Data Base will facilitate our understanding of the factors associated with graft recurrence.
II. EXPANDED CRITERIA FOR LIVER TRANSPLANT FOR HEPATOCELLULAR CARCINOMA
We have redefined the criteria for liver transplantation beyond the Milan criteria. The UCSF criteria enables additional patients to benefit from liver transplants without compromising outcome.
Research & Funding
Data provided by UCSF Profiles, powered by CTSI
- LIVER TRANSPLANTATION CENTERSSponsor: NIH/NIDDKSponsor ID: N01DK002252Funding Period:Jan 1990-Dec 1997Principal Investigator
- ALLOGRAFT RESPONSE TO LIVER TISSUESponsor: NIH/NIAIDSponsor ID: R01AI028284Funding Period:Sep 1988-Sep 1995Principal Investigator
- ORGAN TRANSPLANTS: ANALYSIS OF MIGRATING LYMPHOCYTESSponsor: NIH/NIAIDSponsor ID: R23AI021560Funding Period:Jul 1984-Jun 1987Principal Investigator
Publications
MOST RECENT PUBLICATIONS FROM A TOTAL OF 424
Data provided by UCSF Profiles, powered by CTSI
- Chadha R, Sakai T, Rajakumar A, Shingina A, Yoon U, Patel D, Spiro M, Bhangui P, Sun LY, Humar A, Bezinover D, Findlay J, Saigal S, Singh S, Yi NJ, Rodriguez-Davalos M, Kumar L, Kumaran V, Agarwal S, Berlakovich G, Egawa H, Lerut J, Clemens Broering D, Berenguer M, Cattral M, Clavien PA, Chen CL, Shah S, Zhu ZJ, Ascher N, Bhangui P, Rammohan A, Emond J, Rela M. Anesthesia and Critical Care for the Prediction and Prevention for Small-for-size Syndrome: Guidelines from the ILTS-iLDLT-LTSI Consensus Conference. Transplantation. 2023 10 01; 107(10):2216-2225. View in PubMed
- Kow AWC, Liu J, Patel MS, De Martin E, Reddy MS, Soejima Y, Syn N, Watt K, Xia Q, Saraf N, Kamel R, Nasralla D, McKenna G, Srinvasan P, Elsabbagh AM, Pamecha V, Palaniappan K, Mas V, Tokat Y, Asthana S, Cherukuru R, Egawa H, Lerut J, Broering D, Berenguer M, Cattral M, Clavien PA, Chen CL, Shah S, Zhu ZJ, Emond J, Ascher N, Rammohan A, Bhangui P, Rela M, Kim DS, Ikegami T, ILTS-iLDLT-LTSI SFSS Working Group. Post Living Donor Liver Transplantation Small-for-size Syndrome: Definitions, Timelines, Biochemical, and Clinical Factors for Diagnosis: Guidelines From the ILTS-iLDLT-LTSI Consensus Conference. Transplantation. 2023 10 01; 107(10):2226-2237. View in PubMed
- Kirchner VA, Shankar S, Victor DW, Tanaka T, Goldaracena N, Troisi RI, Olthoff KM, Kim JM, Pomfret EA, Heaton N, Polak WG, Shukla A, Mohanka R, Balci D, Ghobrial M, Gupta S, Maluf D, Fung JJ, Eguchi S, Roberts J, Eghtesad B, Selzner M, Prasad R, Kasahara M, Egawa H, Lerut J, Broering D, Berenguer M, Cattral MS, Clavien PA, Chen CL, Shah SR, Zhu ZJ, Ascher N, Ikegami T, Bhangui P, Rammohan A, Emond JC, Rela M. Management of Established Small-for-size Syndrome in Post Living Donor Liver Transplantation: Medical, Radiological, and Surgical Interventions: Guidelines From the ILTS-iLDLT-LTSI Consensus Conference. Transplantation. 2023 10 01; 107(10):2238-2246. View in PubMed
- Meier RPH, Nunez M, Syed SM, Feng S, Tavakol M, Freise CE, Roberts JP, Ascher NL, Hirose R, Roll GR. DCD liver transplant in patients with a MELD over 35. Front Immunol. 2023; 14:1246867. View in PubMed
- Hakeem AR, Mathew JS, Aunés CV, Mazzola A, Alconchel F, Yoon YI, Testa G, Selzner N, Sarin SK, Lee KW, Soin A, Pomposelli J, Menon K, Goyal N, Kota V, Abu-Gazala S, Rodriguez-Davalos M, Rajalingam R, Kapoor D, Durand F, Kamath P, Jothimani D, Sudhindran S, Vij V, Yoshizumi T, Egawa H, Lerut J, Broering D, Berenguer M, Cattral M, Clavien PA, Chen CL, Shah S, Zhu ZJ, Ascher N, Bhangui P, Rammohan A, Emond J, Rela M. Preventing Small-for-size Syndrome in Living Donor Liver Transplantation: Guidelines From the ILTS-iLDLT-LTSI Consensus Conference. Transplantation. 2023 10 01; 107(10):2203-2215. View in PubMed
- View All Publications
Videos
Data provided by UCSF Profiles, powered by CTSI
- Transplantation: The Cerberus of the 21st Century
- UCSF 2010 Liver Transplant Update: Extending the Indications for Live Donor Liver Transplants
- Liver Transplantation: Prometheus’ Promise; The Liver Cancer Epidemic: A Major Health Problem Worldwide
- The UCSF Liver Transplant and Hepatobiliary Surgery Program
In the News
- - December 09, 2020UCSF Transplant Surgery's Dr. Nancy Ascher, is profiled in a four part documentary series produced by BBC Studios' The Science Unit will premiere globally December 9 2020 on Netflix. The Surgeon's Cut profiles four ground-breaking surgeons from around the world, each with a visionary approach to their craft. "They're philosophers, storytellers and pioneers in their fields. Four surgeons reflect on their lives and professions in this inspiring docuseries." The documentary profiles Dr. [...]
- UCSF General Surgery Residency Program - Alexi Callen - November 16, 2020Hillary Braun, M.D., a general surgery research resident, was recently named to the Declaration of Istanbul Custodian Group (DICG). The DICG is an international organization of transplant professionals whose purpose is to "promote, implement and uphold the Declaration of Istanbul so as to combat organ trafficking, transplant tourism and transplant commercialism and to encourage adoption of effective and ethical transplantation practices around the world". Dr. Braun's research time has been [...]

- UCSF General Surgery Residency Program - Alexi Callen - October 16, 2020Hillary Braun, M.D., a general surgery research resident, was named the 2020 Bruce A. Luxon Emerging Liver Scholar by the American Association for the Study of Liver Diseases (AASLD). The Emerging Liver Scholars program selects 20 medicine or surgery residents who are interested in the study of liver diseases to participate in a curated program at the AASLD's annual Liver Meeting, which will be held virtually this year November 13-16, 2020. In addition to participation in the Emerging Liver [...]

- UCSF School of Medicine - Communications Team - May 19, 2020Nancy Ascher, M.D., Ph.D., world-renowned organ transplant surgeon and a former Chair of the Department of Surgery, received the Holly Smith Award for Exceptional Service to the School of Medicine for 2020. The award, now in its 21st year, recognizes exceptional service to the School of Medicine. It is the school's most prestigious award, and provides an opportunity to celebrate our colleagues who embody the qualities and contributions exemplified by Holly Smith, MD, professor emeritus and [...]

- Washington Post - Lenny Bernstein - May 11, 2019Just 42 years old, Erosalyn Deveza was drifting toward death. Her kidneys were barely functioning. She was constantly exhausted. She had vertigo and vomited frequently. She was tethered to a home dialysis machine for eight hours each night as she slept. A kidney transplant was the only thing that could save her, but it was unlikely to happen in time in the United States. No one on Deveza's side of the family could provide an organ through a living donation, doctors said, because all were at [...]

- UCSF Transplant Surgery - Richard Barg - July 10, 2018Nancy Ascher, M.D., Ph.D., the world-renowned organ transplant surgeon and a former Chair of the UCSF Department of Surgery, has also been invited to serve on the WHO Task Force on Donation and Transplantation of Human Organs and Tissues, an international multidisciplinary task force of 31 experts spanning the fields of medicine, surgery, ethics, law, patients' rights, public administration and health systems. The task force is charged with establishing the fundamentals of ethical [...]
- UCSF Transplant Surgery - October 16, 2015UCSF News reports on the celebration of Diversity Month 2015 at UCSF and the award of the Chancellor Diversity Award for the Advancement of Women to Nancy L. Ascher, M.D., Ph.D.: Nancy Ascher, MD, has been chair of the UCSF Department of Surgery for the past 16 years. Ascher completed her undergraduate and medical education at the University of Michigan, Ann Arbor. She completed a general surgery residency and clinical transplantation fellowship at the University of Minnesota after which she [...]

- UCSF Transplant Surgery - December 20, 2014A new video on AASLD TV (American Association for the Study of Liver Diseases) features the UCSF Liver Transplant Program and faculty John P. Roberts, M.D., Norah A. Terrault, M.D., M.P.H. and Francis Y.K. Yao, M.D. As a leader in the treatment of liver disease and transplantation, UCSF has performed more than 2,500 liver transplants in both children and adults, many in their growing living donor liver transplantation program. The UCSF team is also researching cures for hepatitis as well as [...]

- UCSF Department of Surgery - August 08, 2013"This issue of Inside Surgery highlights the UCSF Lung Transplant Program and the new technology called ex vivo lung perfusion that will help to increase the availability of donor lungs. It also features the Cardiac Transplantation and Mechanical Circulatory Support Program as well as the Pediatric Heart Failure and Pediatric Heart and Lung Transplant Program. Read an update by Nancy Ascher, M.D., Ph.D., chair of the UCSF Department of Surgery.........."

- UCSF Transplant Surgery - June 01, 2013"Dr. (Nancy) Ascher excels in her role as Chair of Surgery, not only for her inexplicable foresight, but because she stays connected to trainees and students. This year, Dr. Ascher received the Francis Moore Excellence in Mentorship in the Field of Transplantation Surgery Award from the American Society of Transplant Surgeons." "Residents and fellows noted that Dr. Nancy Ascher is an effective mentor because she treats them like colleagues and not just trainees. Residents and fellows felt [...]

- UCSF Transplant Surgery - May 30, 2013"It was 1975 when Nancy Ascher, MD, PhD, chose surgery, a specialty shoulder-deep in men. Then again, so was medical school - Ascher was one of 20 women in her class of 180. After her residency, she blew past every gender barrier to become the first woman to perform a liver transplant, garnering enough speed to break through the stainless-steel ceiling to serve as UCSF's first female chair of surgery - one of three women holding that title in the country. The pace at which Ascher propels [...]

- UCSF Department of Surgery - November 08, 2012On November 5th, Captain Chesley B. "Sully" Sullenberger, III spoke to a UCSF audience at Cole Hall on "Leadership in Advancing National Efforts in Patient Safety and Optimal Quality of Care". He was introduced by Hobart W. Harris, M.D., M.P.H., Chief of the Division of General Surgery, who underscored how Sullenberger's aviation experience has informed patient safety and the evolution of modern clinical practice.Captain Sullenberger spoke at the invitation of Nancy L. Ascher, M.D., [...]

- UCSF Transplant Surgery - June 14, 2012Liver cancer patients in need of an organ transplant often face a cruel reality -- while waiting for a deceased-donor liver, their cancer may worsen, spreading to other organs and making them ineligible for a transplant. With two children to raise and time ticking down, Amy Baghdadi was fast running out of options. But at her daughter's soccer practice, a fellow parent, who happened to be UCSF transplant surgeon, Andrew Posselt, M.D., Ph.D., heard Amy's story, and convinced there were other [...]

- UCSF Transplant Surgery - September 22, 2008Nancy Ascher, MD, PhD on NPR's Forum with Michael Krasny Each day in the U.S., 19 people die waiting for donated organs. To help increase supply, some health experts and economists want to legalize the market for human organs. We take up the issue with a panel of experts.

- UCSF Department of Surgery - October 08, 2007Dr. Nancy Ascher and Dr. Holger Willenbring were interviewed by PBS NewsHour correspondent Spencer Michaels about the transformation of embryonic stem cells into new liver cells as a treatment for patients.


- UCSF Transplant Surgery - December 18, 2005"Of all the things for a married couple to bicker about, Nancy Ascher and John Roberts have hit on a first -- a pulsing human liver. To be precise, they are standing forehead to forehead with a man splayed out between them. Roberts wants more of his liver to take next door to a waiting recipient. Ascher wants more of it left behind for the donor's recovery."

Patient Stories
- Gloria & Veronica Ramos
Living Donor Transplant Emblemmatic of Loving Family
UCSF Transplant Surgery - by Sarah Krumholz - September 01, 2006 When Gloria Ramos received the call in August 2000 that UCSF Medical Center had a liver for the transplant she badly needed, the Ramos family drove to the hospital with great anticipation and excitement. But further testing of the available organ revealed it wasn't a good match for Gloria and her daughters and husband expressed their disappointment. "This only means that I'm at the top of the list," Gloria recalls assuring her family. "I'll get called again!" Gloria contracted Hepatitis C through a blood transfusion in 1982 but the deadly virus lived undetected in her body until the summer[...]
When Gloria Ramos received the call in August 2000 that UCSF Medical Center had a liver for the transplant she badly needed, the Ramos family drove to the hospital with great anticipation and excitement. But further testing of the available organ revealed it wasn't a good match for Gloria and her daughters and husband expressed their disappointment. "This only means that I'm at the top of the list," Gloria recalls assuring her family. "I'll get called again!" Gloria contracted Hepatitis C through a blood transfusion in 1982 but the deadly virus lived undetected in her body until the summer[...]
